How You Can Treat Fallen Arches
Overview

The term 'fallen arches' is rather a historical one, but is one many people seem to have heard of. What it essentially refers to is a ligament problem in the sole of his foot where these run along its length. In most people these ligaments provide support to the foot when walking and help keep the foot in a normal anatomical position. Some people however seem to have laxity in these ligaments so the foot becomes under undue strain and pain can occur as a result.
Causes
If you tend to pronate, roll your foot and ankle in when you walk or run you may cause your arch to fall. Pronating your foot and ankle interferes with the normal movement of your foot. You should land on your heel first and roll through the middle of your foot. Landing on the inside of your foot stresses foot and ankle bones, tendons and ligaments. This can lead to many problems including flat feet. Your podiatrist can examine the way you land on your foot and then design orthotics to help you move correctly. It is important to wear the right shoes for an activity, to provide necessary arch support. Making these corrections can relieve symptoms.
Symptoms
A significant number of people with fallen arches (flat feet) experience no pain and have no problems. Some, however, may experience pain in their feet, especially when the connecting ligaments and muscles are strained. The leg joints may also be affected, resulting in pain. If the ankles turn inwards because of flat feet the most likely affected areas will be the feet, ankles and knees. Some people have flat feet because of a developmental fault during childhood, while others may find that the problem develops as they age, or after a pregnancy. There are some simple devices which may prevent the complications of flat feet.
Diagnosis
It is important for people with foot pain to know if they have flat feet. The following tests can help you determine your arch type. When you get out of a swimming pool, look at your footprint on the concrete. The front of the foot will be joined to the heel by a strip. If your foot is flat, then the strip is the same width as the front of the foot, creating a footprint that looks like a stretched out pancake. With a normal arch, the strip is about half the width of the front of the foot. If you have a high arch, only a thin strip connects the front of the foot with the heel. Put your shoes on a flat table and view them at eye level from behind. See if the sole is worn evenly. A flat foot will cause more wear on the inside of the sole, especially in the heel area. The shoe will easily rock side to side. A flat foot will also cause the upper part of the shoe to lean inward over the sole. Both shoes should wear about the same way. If you have pain in one foot, you should make sure you don't have a fallen arch on that side. There are two good tests you can perform at home to detect this problem. Place your fingertips on a wall that you are directly facing and stand on your tiptoes on one foot. If you can't do it, a fallen arch may be the culprit. Stand with your feet parallel. Have someone stand in back of you and look at your feet from behind. You can also do it yourself if you stand with your back to a mirror. Normally, only the pinky toe is visible from behind. If one foot is flatter than the other, the 4th and sometimes the 3rd toe on that foot can also be seen.
What causes pes planus?
Non Surgical Treatment
Most flexible flat feet are asymptomatic, and do not cause pain. In these cases, there is usually no cause for concern, and the condition may be considered a normal human variant. Flat feet were formerly a physical-health reason for service-rejection in many militaries. However, three military studies on asymptomatic adults (see section below), suggest that persons with asymptomatic flat feet are at least as tolerant of foot stress as the population with various grades of arch. Asymptomatic flat feet are no longer a service disqualification in the U.S. military.
Surgical Treatment

Common indications for surgery are cerebral palsy with an equinovalgus foot, to prevent progression and breakdown of the midfoot. Rigid and painful Pes Planus. To prevent progression, eg with a Charcot joint. Tibialis posterior dysfunction, where non-surgical treatment is unsuccessful. Possible surgical procedures include Achilles tendon lengthening. Calcaneal osteotomy, to re-align the hindfoot. Reconstruction of the tibialis posterior tendon. For severe midfoot collapse of the arch, triple arthrodesis may be indicated.
Prevention
Strap the arches into the anatomically correct positions with athletic tape and leave them like this for some time. If the fallen arches are an issue with the muscular structure, this may give the muscles an opportunity to strengthen. This is definitely not a fallen arches cure all the time but it can help prevent it more times than not. Ask a doctor or physical therapists to show you how to do this taping. Find shoes that fit. This may require that you get your foot measured and molded to ensure that the shoe will fit. Shoes that are too big, too tight or too short, may not directly cause the fallen arches, but they can assist with the damage to the area. These shoes should have thick cushioning inside and have plenty of room for your toes. Walk without shoes as much as possible. Shoes directly assist with weakening and distorting the arches of the feet so going without shoes can actually help strengthen your arches and prevent fallen arches. Walking on hard and bumpy surfaces barefooted makes the muscles in your feet strengthen in order to prevent injury. It is a coping mechanism by your body. Insert heel cups or insoles into the shoes that you wear the most. Many people wear uncomfortable shoes to work and these are the same shoes that cause their arches the most problems. Inserting the heel cups and insoles into these shoes can prevent fallen arches from occurring. Many people place these inserts into all their shoes to ensure support. Ask a medical professional, either your doctor or a physical therapist, about daily foot exercises that may keep the arches stronger than normal. Many times, you can find exercises and stretches on the Internet on various websites. Curling your toes tightly and rotating your feet will help strengthen your longitudinal arches. Relax your feet and shake them for a minute or so before you do any arch exercises. This will loosen the muscles in your feet that stay tight due to normal daily activities. Wear rigid soled sandals whenever possible to provide a strong support for your arches. Wooden soled sandals are the best ones if available. Walk or jog on concrete as much as you can. This will create a sturdy support for your arches. Running or walking in sandy areas or even on a treadmill, does not give rigid support. Instead, these surfaces absorb the step, offering no support for arches.

The term 'fallen arches' is rather a historical one, but is one many people seem to have heard of. What it essentially refers to is a ligament problem in the sole of his foot where these run along its length. In most people these ligaments provide support to the foot when walking and help keep the foot in a normal anatomical position. Some people however seem to have laxity in these ligaments so the foot becomes under undue strain and pain can occur as a result.
Causes
If you tend to pronate, roll your foot and ankle in when you walk or run you may cause your arch to fall. Pronating your foot and ankle interferes with the normal movement of your foot. You should land on your heel first and roll through the middle of your foot. Landing on the inside of your foot stresses foot and ankle bones, tendons and ligaments. This can lead to many problems including flat feet. Your podiatrist can examine the way you land on your foot and then design orthotics to help you move correctly. It is important to wear the right shoes for an activity, to provide necessary arch support. Making these corrections can relieve symptoms.
Symptoms
A significant number of people with fallen arches (flat feet) experience no pain and have no problems. Some, however, may experience pain in their feet, especially when the connecting ligaments and muscles are strained. The leg joints may also be affected, resulting in pain. If the ankles turn inwards because of flat feet the most likely affected areas will be the feet, ankles and knees. Some people have flat feet because of a developmental fault during childhood, while others may find that the problem develops as they age, or after a pregnancy. There are some simple devices which may prevent the complications of flat feet.
Diagnosis
It is important for people with foot pain to know if they have flat feet. The following tests can help you determine your arch type. When you get out of a swimming pool, look at your footprint on the concrete. The front of the foot will be joined to the heel by a strip. If your foot is flat, then the strip is the same width as the front of the foot, creating a footprint that looks like a stretched out pancake. With a normal arch, the strip is about half the width of the front of the foot. If you have a high arch, only a thin strip connects the front of the foot with the heel. Put your shoes on a flat table and view them at eye level from behind. See if the sole is worn evenly. A flat foot will cause more wear on the inside of the sole, especially in the heel area. The shoe will easily rock side to side. A flat foot will also cause the upper part of the shoe to lean inward over the sole. Both shoes should wear about the same way. If you have pain in one foot, you should make sure you don't have a fallen arch on that side. There are two good tests you can perform at home to detect this problem. Place your fingertips on a wall that you are directly facing and stand on your tiptoes on one foot. If you can't do it, a fallen arch may be the culprit. Stand with your feet parallel. Have someone stand in back of you and look at your feet from behind. You can also do it yourself if you stand with your back to a mirror. Normally, only the pinky toe is visible from behind. If one foot is flatter than the other, the 4th and sometimes the 3rd toe on that foot can also be seen.
What causes pes planus?
Non Surgical Treatment
Most flexible flat feet are asymptomatic, and do not cause pain. In these cases, there is usually no cause for concern, and the condition may be considered a normal human variant. Flat feet were formerly a physical-health reason for service-rejection in many militaries. However, three military studies on asymptomatic adults (see section below), suggest that persons with asymptomatic flat feet are at least as tolerant of foot stress as the population with various grades of arch. Asymptomatic flat feet are no longer a service disqualification in the U.S. military.
Surgical Treatment

Common indications for surgery are cerebral palsy with an equinovalgus foot, to prevent progression and breakdown of the midfoot. Rigid and painful Pes Planus. To prevent progression, eg with a Charcot joint. Tibialis posterior dysfunction, where non-surgical treatment is unsuccessful. Possible surgical procedures include Achilles tendon lengthening. Calcaneal osteotomy, to re-align the hindfoot. Reconstruction of the tibialis posterior tendon. For severe midfoot collapse of the arch, triple arthrodesis may be indicated.
Prevention
Strap the arches into the anatomically correct positions with athletic tape and leave them like this for some time. If the fallen arches are an issue with the muscular structure, this may give the muscles an opportunity to strengthen. This is definitely not a fallen arches cure all the time but it can help prevent it more times than not. Ask a doctor or physical therapists to show you how to do this taping. Find shoes that fit. This may require that you get your foot measured and molded to ensure that the shoe will fit. Shoes that are too big, too tight or too short, may not directly cause the fallen arches, but they can assist with the damage to the area. These shoes should have thick cushioning inside and have plenty of room for your toes. Walk without shoes as much as possible. Shoes directly assist with weakening and distorting the arches of the feet so going without shoes can actually help strengthen your arches and prevent fallen arches. Walking on hard and bumpy surfaces barefooted makes the muscles in your feet strengthen in order to prevent injury. It is a coping mechanism by your body. Insert heel cups or insoles into the shoes that you wear the most. Many people wear uncomfortable shoes to work and these are the same shoes that cause their arches the most problems. Inserting the heel cups and insoles into these shoes can prevent fallen arches from occurring. Many people place these inserts into all their shoes to ensure support. Ask a medical professional, either your doctor or a physical therapist, about daily foot exercises that may keep the arches stronger than normal. Many times, you can find exercises and stretches on the Internet on various websites. Curling your toes tightly and rotating your feet will help strengthen your longitudinal arches. Relax your feet and shake them for a minute or so before you do any arch exercises. This will loosen the muscles in your feet that stay tight due to normal daily activities. Wear rigid soled sandals whenever possible to provide a strong support for your arches. Wooden soled sandals are the best ones if available. Walk or jog on concrete as much as you can. This will create a sturdy support for your arches. Running or walking in sandy areas or even on a treadmill, does not give rigid support. Instead, these surfaces absorb the step, offering no support for arches.
Functional Leg-Length Discrepancy
Overview
Every person?s body is unique and will show different symptoms due to a short leg. Athletes are able to distinguish the negative effects of a leg length that is just 3 mm shorter then the other. A whole host of negative effects can occur to the body that can create chronic pain and may necessitate surgical interventions. The effect of a short leg can be seen almost everywhere in the body.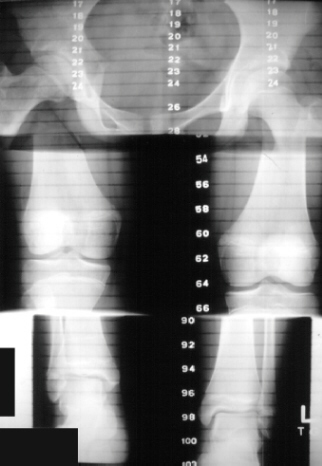
Causes
A number of causes may lead to leg length discrepancy in children. Differences in leg length frequently follow fractures in the lower extremities in children due to over or under stimulation of the growth plates in the broken leg. Leg length discrepancy may also be caused by a congenital abnormality associated with a condition called hemihypertrophy. Or it may result from neuromuscular diseases such as polio and cerebral palsy. Many times, no cause can be identified. A small leg length discrepancy of a quarter of an inch or less is quite common in the general population and of no clinical significance. Larger leg length discrepancies become more significant. The long-term consequences of a short leg may include knee pain, back pain, and abnormal gait or limp.
Symptoms
The effects of a short leg depend upon the individual and the extent of discrepancy. The most common manifestation if a lateral deviation of the lumbar spine toward the short side with compensatory curves up the spine that can extend into the neck and even impacts the TMJ. Studies have shown that anterior and posterior curve abnormalities also can result.
Diagnosis
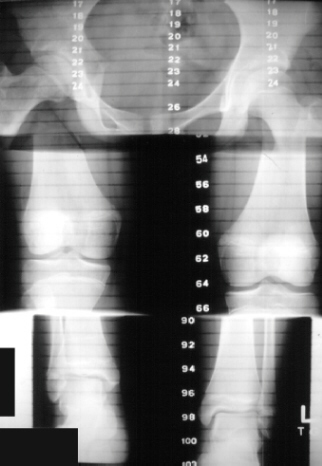
Leg length discrepancy may be diagnosed during infancy or later in childhood, depending on the cause. Conditions such as hemihypertrophy or hemiatrophy are often diagnosed following standard newborn or infant examinations by a pediatrician, or anatomical asymmetries may be noticed by a child's parents. For young children with hemihypertophy as the cause of their LLD, it is important that they receive an abdominal ultrasound of the kidneys to insure that Wilm's tumor, which can lead to hypertrophy in the leg on the same side, is not present. In older children, LLD is frequently first suspected due to the emergence of a progressive limp, warranting a referral to a pediatric orthopaedic surgeon. The standard workup for LLD is a thorough physical examination, including a series of measurements of the different portions of the lower extremities with the child in various positions, such as sitting and standing. The orthopaedic surgeon will observe the child while walking and performing other simple movements or tasks, such as stepping onto a block. In addition, a number of x-rays of the legs will be taken, so as to make a definitive diagnosis and to assist with identification of the possible etiology (cause) of LLD. Orthopaedic surgeons will compare x-rays of the two legs to the child's age, so as to assess his/her skeletal age and to obtain a baseline for the possibility of excessive growth rate as a cause. A growth chart, which compares leg length to skeletal age, is a simple but essential tool used over time to track the progress of the condition, both before and after treatment. Occasionally, a CT scan or MRI is required to further investigate suspected causes or to get more sophisticated radiological pictures of bone or soft tissue.
Non Surgical Treatment
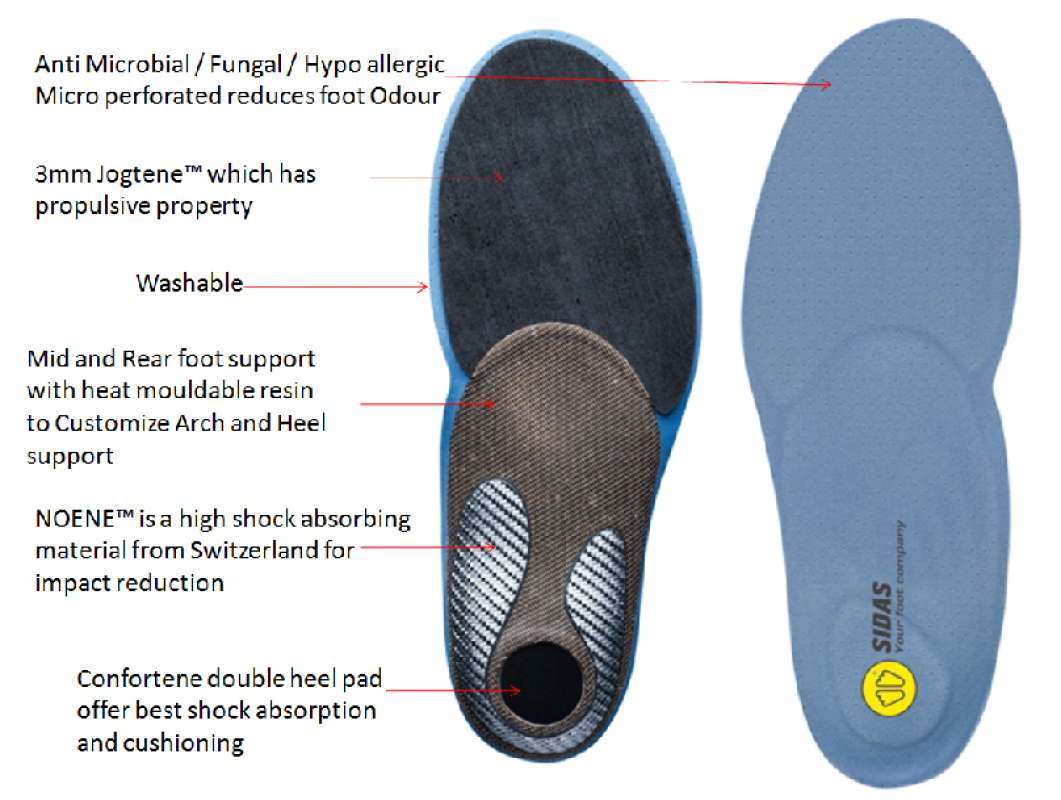
Internal heel lifts: Putting a simple heel lift inside the shoe or onto a foot orthotic has the advantage of being transferable to many pairs of shoes. It is also aesthetically more pleasing as the lift remains hidden from view. However, there is a limit as to how high the lift can be before affecting shoe fit. Dress shoes will usually only accommodate small lifts (1/8"1/4") before the heel starts to piston out of the shoe. Sneakers and workboots may allow higher lifts, e.g., up to 1/2", before heel slippage problems arise. External heel lifts: If a lift of greater than 1/2" is required, you should consider adding to the outsole of the shoe. In this way, the shoe fit remains good. Although some patients may worry about the cosmetics of the shoe, it does ensure better overall function. Nowadays with the development of synthetic foams and crepes, such lifts do not have to be as heavy as the cork buildups of the past. External buildups are not transferable and they will wear down over time, so the patient will need to be vigilant in having them repaired. On ladies' high-heel shoes, it may be possible to lower one heel and thereby correct the imbalance.

shoe lift inserts
Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
Every person?s body is unique and will show different symptoms due to a short leg. Athletes are able to distinguish the negative effects of a leg length that is just 3 mm shorter then the other. A whole host of negative effects can occur to the body that can create chronic pain and may necessitate surgical interventions. The effect of a short leg can be seen almost everywhere in the body.
Causes
A number of causes may lead to leg length discrepancy in children. Differences in leg length frequently follow fractures in the lower extremities in children due to over or under stimulation of the growth plates in the broken leg. Leg length discrepancy may also be caused by a congenital abnormality associated with a condition called hemihypertrophy. Or it may result from neuromuscular diseases such as polio and cerebral palsy. Many times, no cause can be identified. A small leg length discrepancy of a quarter of an inch or less is quite common in the general population and of no clinical significance. Larger leg length discrepancies become more significant. The long-term consequences of a short leg may include knee pain, back pain, and abnormal gait or limp.
Symptoms
The effects of a short leg depend upon the individual and the extent of discrepancy. The most common manifestation if a lateral deviation of the lumbar spine toward the short side with compensatory curves up the spine that can extend into the neck and even impacts the TMJ. Studies have shown that anterior and posterior curve abnormalities also can result.
Diagnosis
Leg length discrepancy may be diagnosed during infancy or later in childhood, depending on the cause. Conditions such as hemihypertrophy or hemiatrophy are often diagnosed following standard newborn or infant examinations by a pediatrician, or anatomical asymmetries may be noticed by a child's parents. For young children with hemihypertophy as the cause of their LLD, it is important that they receive an abdominal ultrasound of the kidneys to insure that Wilm's tumor, which can lead to hypertrophy in the leg on the same side, is not present. In older children, LLD is frequently first suspected due to the emergence of a progressive limp, warranting a referral to a pediatric orthopaedic surgeon. The standard workup for LLD is a thorough physical examination, including a series of measurements of the different portions of the lower extremities with the child in various positions, such as sitting and standing. The orthopaedic surgeon will observe the child while walking and performing other simple movements or tasks, such as stepping onto a block. In addition, a number of x-rays of the legs will be taken, so as to make a definitive diagnosis and to assist with identification of the possible etiology (cause) of LLD. Orthopaedic surgeons will compare x-rays of the two legs to the child's age, so as to assess his/her skeletal age and to obtain a baseline for the possibility of excessive growth rate as a cause. A growth chart, which compares leg length to skeletal age, is a simple but essential tool used over time to track the progress of the condition, both before and after treatment. Occasionally, a CT scan or MRI is required to further investigate suspected causes or to get more sophisticated radiological pictures of bone or soft tissue.
Non Surgical Treatment
Internal heel lifts: Putting a simple heel lift inside the shoe or onto a foot orthotic has the advantage of being transferable to many pairs of shoes. It is also aesthetically more pleasing as the lift remains hidden from view. However, there is a limit as to how high the lift can be before affecting shoe fit. Dress shoes will usually only accommodate small lifts (1/8"1/4") before the heel starts to piston out of the shoe. Sneakers and workboots may allow higher lifts, e.g., up to 1/2", before heel slippage problems arise. External heel lifts: If a lift of greater than 1/2" is required, you should consider adding to the outsole of the shoe. In this way, the shoe fit remains good. Although some patients may worry about the cosmetics of the shoe, it does ensure better overall function. Nowadays with the development of synthetic foams and crepes, such lifts do not have to be as heavy as the cork buildups of the past. External buildups are not transferable and they will wear down over time, so the patient will need to be vigilant in having them repaired. On ladies' high-heel shoes, it may be possible to lower one heel and thereby correct the imbalance.

shoe lift inserts
Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
Addressing Mortons Neuroma
Overview
 Morton's neuroma, also called Morton's metatarsalgia, Morton's disease, Morton's neuralgia, Morton metatarsalgia, Morton nerve entrapment, plantar neuroma, or intermetatarsal neuroma is a benign (non-cancerous) growth of nerve tissue (neuroma) that develops in the foot, usually between the third and fourth toes (an intermetatarsal plantar nerve, most commonly of the third and fourth intermetatarsal spaces). It is a common, painful condition.
Morton's neuroma, also called Morton's metatarsalgia, Morton's disease, Morton's neuralgia, Morton metatarsalgia, Morton nerve entrapment, plantar neuroma, or intermetatarsal neuroma is a benign (non-cancerous) growth of nerve tissue (neuroma) that develops in the foot, usually between the third and fourth toes (an intermetatarsal plantar nerve, most commonly of the third and fourth intermetatarsal spaces). It is a common, painful condition.
Causes
The exact cause is unknown. Doctors believe the following may play a role in the development of this condition. Wearing tight shoes and high heels. Abnormal positioning of toes. Flat feet. Forefoot problems, including bunions and hammer toes. High foot arches. Morton neuroma is more common in women than in men.
Symptoms
Many patients describe the sensation as a burning pain in the ball of the foot that often radiates to the toes. Initially, the pain may become much more apparent when the person wears tight, narrow or high-heeled shoes, or engages in activities which place pressure on the foot. Eventually, symptoms may be continuous and last for days, and even weeks. MRI (magnetic resonance imaging) scans have revealed Morton's neuroma lesions in patients who had no symptoms at all. Symptoms can become so disrupting that many affected individuals become anxious about walking, or even placing their foot on the ground.
Diagnosis
Podiatrists conduct a physical examination and may order imaging tests, such as x-ray or MRI scan to diagnose Morton's neuroma. Conservative treatment options include custom-fitted orthotics, medication, and/or alcohol injections designed to harden the nerve. However, most patients with Morton's neuroma need minor surgery.
Non Surgical Treatment
Nonsurgical treatment is tried first. Your doctor may recommend any of the following. Padding and taping the toe area, shoe inserts, changes to footwear, for example wearing shoes with wider toe boxes or flat heels, Anti-inflammatory medicines taken by mouth or injected into the toe area, nerve blocking medicines injected into the toe area, other painkillers, physical therapy. Anti-inflammatories and painkillers are not recommended for long-term treatment. In some cases, surgery is needed to remove the thickened tissue and inflammed nerve. This helps relieve pain and improve foot function. Numbness after surgery is permanent.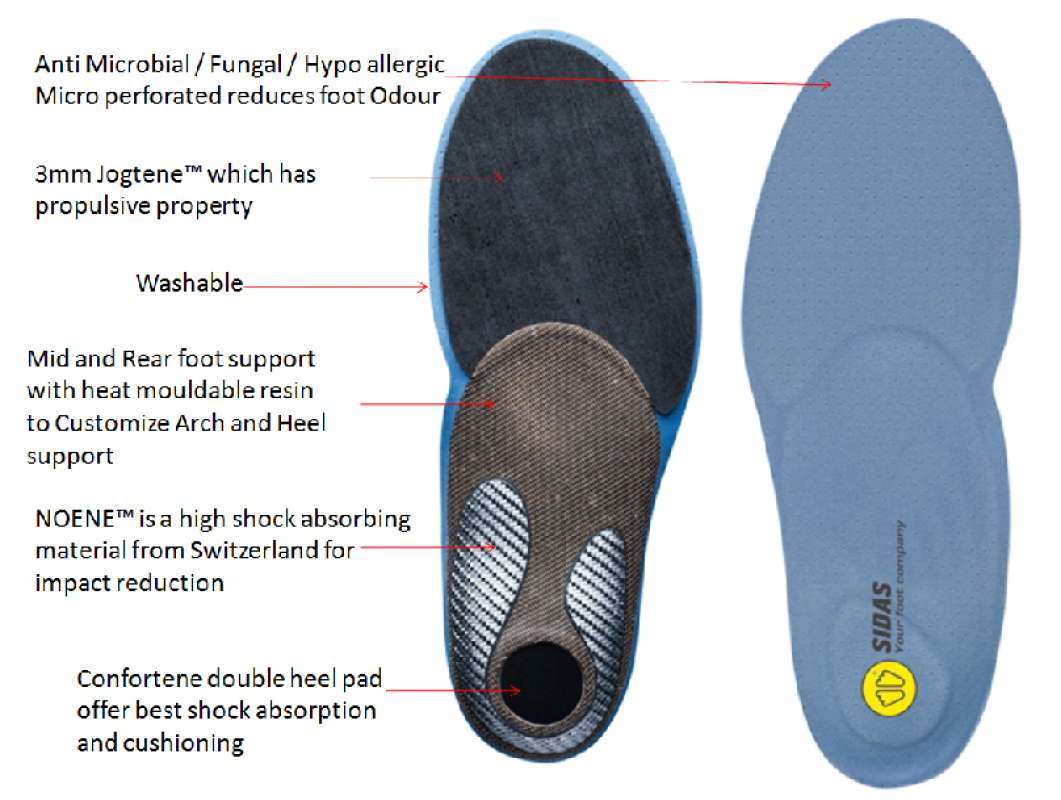
Surgical Treatment
Interdigital neurectomy (removal of the diseased nerve) in right hands, should give satisfactory results almost all the time. Some of the reasons behind failure is when not enough nerve is dissected, mistakes in initial diagnosis, or bad handling of adjacent nerves, tendons and joint capsules during the operation. It is very common and acceptable to have some numbness in the area where the nerve used to be. This never causes any discomfort and often gets better in few years. It is crucial to address the biomechanical pathologies underlying the impingement of the nerve during and after the surgery.
Prevention
Wearing shoes that fit properly and that have plenty of room in the toe area may help prevent Morton's neuroma.
 Morton's neuroma, also called Morton's metatarsalgia, Morton's disease, Morton's neuralgia, Morton metatarsalgia, Morton nerve entrapment, plantar neuroma, or intermetatarsal neuroma is a benign (non-cancerous) growth of nerve tissue (neuroma) that develops in the foot, usually between the third and fourth toes (an intermetatarsal plantar nerve, most commonly of the third and fourth intermetatarsal spaces). It is a common, painful condition.
Morton's neuroma, also called Morton's metatarsalgia, Morton's disease, Morton's neuralgia, Morton metatarsalgia, Morton nerve entrapment, plantar neuroma, or intermetatarsal neuroma is a benign (non-cancerous) growth of nerve tissue (neuroma) that develops in the foot, usually between the third and fourth toes (an intermetatarsal plantar nerve, most commonly of the third and fourth intermetatarsal spaces). It is a common, painful condition.Causes
The exact cause is unknown. Doctors believe the following may play a role in the development of this condition. Wearing tight shoes and high heels. Abnormal positioning of toes. Flat feet. Forefoot problems, including bunions and hammer toes. High foot arches. Morton neuroma is more common in women than in men.
Symptoms
Many patients describe the sensation as a burning pain in the ball of the foot that often radiates to the toes. Initially, the pain may become much more apparent when the person wears tight, narrow or high-heeled shoes, or engages in activities which place pressure on the foot. Eventually, symptoms may be continuous and last for days, and even weeks. MRI (magnetic resonance imaging) scans have revealed Morton's neuroma lesions in patients who had no symptoms at all. Symptoms can become so disrupting that many affected individuals become anxious about walking, or even placing their foot on the ground.
Diagnosis
Podiatrists conduct a physical examination and may order imaging tests, such as x-ray or MRI scan to diagnose Morton's neuroma. Conservative treatment options include custom-fitted orthotics, medication, and/or alcohol injections designed to harden the nerve. However, most patients with Morton's neuroma need minor surgery.
Non Surgical Treatment
Nonsurgical treatment is tried first. Your doctor may recommend any of the following. Padding and taping the toe area, shoe inserts, changes to footwear, for example wearing shoes with wider toe boxes or flat heels, Anti-inflammatory medicines taken by mouth or injected into the toe area, nerve blocking medicines injected into the toe area, other painkillers, physical therapy. Anti-inflammatories and painkillers are not recommended for long-term treatment. In some cases, surgery is needed to remove the thickened tissue and inflammed nerve. This helps relieve pain and improve foot function. Numbness after surgery is permanent.
Surgical Treatment
Interdigital neurectomy (removal of the diseased nerve) in right hands, should give satisfactory results almost all the time. Some of the reasons behind failure is when not enough nerve is dissected, mistakes in initial diagnosis, or bad handling of adjacent nerves, tendons and joint capsules during the operation. It is very common and acceptable to have some numbness in the area where the nerve used to be. This never causes any discomfort and often gets better in few years. It is crucial to address the biomechanical pathologies underlying the impingement of the nerve during and after the surgery.
Prevention
Wearing shoes that fit properly and that have plenty of room in the toe area may help prevent Morton's neuroma.
For Leg Length Difference Chiropodists Prefer Shoe Lifts
There are actually not one but two unique variations of leg length discrepancies, congenital and acquired. Congenital means you are born with it. One leg is structurally shorter than the other. Through developmental periods of aging, the human brain senses the step pattern and identifies some variance. Our bodies usually adapts by dipping one shoulder over to the "short" side. A difference of less than a quarter inch isn't really uncommon, require Shoe Lifts to compensate and typically doesn't have a profound effect over a lifetime.

Leg length inequality goes mainly undiagnosed on a daily basis, however this issue is very easily solved, and can eradicate many incidents of back ache.
Treatment for leg length inequality typically consists of Shoe Lifts. Many are economical, usually being below twenty dollars, in comparison to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is the most common health problem afflicting people today. Over 80 million men and women suffer from back pain at some stage in their life. It's a problem that costs businesses millions year after year because of lost time and productivity. New and better treatment methods are always sought after in the hope of lowering economic influence this issue causes.

Men and women from all corners of the earth suffer from foot ache due to leg length discrepancy. In these situations Shoe Lifts can be of beneficial. The lifts are capable of alleviating any pain and discomfort in the feet. Shoe Lifts are recommended by many experienced orthopaedic doctors.
So that they can support the body in a nicely balanced manner, feet have got a crucial function to play. Irrespective of that, it can be the most neglected area in the body. Many people have flat-feet meaning there may be unequal force placed on the feet. This will cause other body parts like knees, ankles and backs to be impacted too. Shoe Lifts guarantee that correct posture and balance are restored.

Leg length inequality goes mainly undiagnosed on a daily basis, however this issue is very easily solved, and can eradicate many incidents of back ache.
Treatment for leg length inequality typically consists of Shoe Lifts. Many are economical, usually being below twenty dollars, in comparison to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is the most common health problem afflicting people today. Over 80 million men and women suffer from back pain at some stage in their life. It's a problem that costs businesses millions year after year because of lost time and productivity. New and better treatment methods are always sought after in the hope of lowering economic influence this issue causes.

Men and women from all corners of the earth suffer from foot ache due to leg length discrepancy. In these situations Shoe Lifts can be of beneficial. The lifts are capable of alleviating any pain and discomfort in the feet. Shoe Lifts are recommended by many experienced orthopaedic doctors.
So that they can support the body in a nicely balanced manner, feet have got a crucial function to play. Irrespective of that, it can be the most neglected area in the body. Many people have flat-feet meaning there may be unequal force placed on the feet. This will cause other body parts like knees, ankles and backs to be impacted too. Shoe Lifts guarantee that correct posture and balance are restored.
Learn How To Identify Heel Spur

Overview
A heel spur is a hook that can form on the calcaneus (heel bone) and can also be related to plantar fasciitis (inflammation of the tissue in the foot?s arch). People who have plantar fasciitis often develop heel spurs. Middle-aged men and women are more prone to heels spurs, but all age groups can be afflicted. Heel spurs can be found through an x-ray, revealing a protruding hook where the plantar fascia is located.
Causes
Heel spurs can form as a result of repeated strain placed on foot muscles and ligaments as well as from abnormally stretching the band of tissue connecting the heel and ball of the foot. Repeated injury to the membrane that lines the heel bone can also cause problems as can repeated tight pressure on the back of the heel. The causes can range from excessive walking (especially if unaccustomed to walking), running or jumping to improperly fitted or worn-out shoes. Runners, volleyball players, and tennis players, people who do step aerobics or stair climbing for exercise, those with flat feet, pregnant women, the obese and diabetics and those who wear tight-fitting shoes with a high heel are all prone to developing spurs (and plantar fasciitis) more readily.

Symptoms
The spur itself is not painful, however, if it is sharp and pointed it can poke into soft tissue surrounding the spur itself. As the bone spur irritates the tissue, inflammation and bruising can occur leading to heel pain. Heel spurs can affect your ability to do your usual work and/or activities, and can also trap and irritate the nerves in your heel area. They can change the way you walk, and can lead to knee, hip and low back injuries. If severe, they may require medical intervention.
Diagnosis
Your doctor, when diagnosing and treating this condition will need an x-ray and sometimes a gait analysis to ascertain the exact cause of this condition. If you have pain in the bottom of your foot and you do not have diabetes or a vascular problem, some of the over-the-counter anti-inflammatory products such as Advil or Ibuprofin are helpful in eradicating the pain. Pain creams, such as Neuro-eze, BioFreeze & Boswella Cream can help to relieve pain and help increase circulation.
Non Surgical Treatment
Common and effective treatments for Heel Spurs include: Stretching exercises, changing to specific shoes, taping or strapping to rest stressed muscles and tendons, custom orthotic devices and physiotherapy. There are many things you can do to treat heel spurs. You should stretch the muscles and ligaments around the area regularly and ensure you are wearing the right footwear for your feet. There are also tapes and straps that you can apply to the muscles and tendons around the area. For more severe cases, custom orthotics may be the way to go along with aggressive physiotherapy. To treat the pain, over the counter NSAIDs (anti-inflammatory medications) is recommended, but use with caution as prolonged use can lead to the development of ulcers. It is therefore best to apply a topical treatment such as Zax?s Original Heelspur Cream, which contains natural ingredients proven to reduce pain and inflammation. More severe forms of the condition may require corticosteroid injections or surgical procedures, but these are very rare cases. Still, should pain become worse and persist, you should consult with your doctor.
Surgical Treatment
In a small number of cases (usually less than 5 percent), patients may not experience relief after trying the recommendations listed above. It is important that conservative treatments (such as those listed above) be performed for AT LEAST a year before considering surgery. Time is important in curing the pain from heel spurs, and insufficient treatment before surgery may subject you to potential complications from the procedure. If these treatments fail, your doctor may consider an operation to loosen the plantar fascia, called a plantar fascia release.
Prevention
You can prevent heel spurs by wearing well-fitting shoes with shock-absorbent soles, rigid shanks, and supportive heel counters; choosing appropriate shoes for each physical activity; warming up and doing stretching exercises before each activity; and pacing yourself during the activities. Avoid wearing shoes with excessive wear on the heels and soles. If you are overweight, losing weight may also help prevent heel spurs.
Techniques To Treat Heel Spur

Overview
Heel spurs are abnormal bony growths that develop at the back of or under the heel. Inflammation around a spur, more so than the spur itself, can cause significant pain. Fortunately, symptoms can be eased with non-surgical treatments for the vast majority of people.
Causes
Over-pronation (flat feet) is a common cause of heel spurs, but people with unusually high arches (pes cavus) can also develop heel spurs. Women have a significantly higher incidence of heel spurs due to the types of footwear often worn on a regular basis.

Symptoms
An individual with the lower legs turning inward, a condition called genu valgus or "knock knees," can have a tendency toward excessive pronation. This can lead to a fallen arch and problems with the plantar fascia and heel spurs. Women tend to suffer from this condition more than men. Heel spurs can also result from an abnormally high arch. Other factors leading to heel spurs include a sudden increase in daily activities, an increase in weight, or a thinner cushion on the bottom of the heel due to old age. A significant increase in training intensity or duration may cause inflammation of the plantar fascia. High-heeled shoes, improperly fitted shoes, and shoes that are too flexible in the middle of the arch or bend before the toe joints will cause problems with the plantar fascia and possibly lead to heel spurs.
Diagnosis
Heel spurs and plantar fasciitis are diagnosed based on the history of pain and tenderness localized to these areas. They are specifically identified when there is point tenderness at the bottom of the heel, which makes it difficult to walk barefoot on tile or wood floors. X-ray examination of the foot is used to identify the bony prominence (spur) of the heel bone (calcaneus).
Non Surgical Treatment
Heel spurs and plantar fascitis are usually controlled with conservative treatment. Early intervention includes stretching the calf muscles while avoiding re-injuring the plantar fascia. Decreasing or changing activities, losing excess weight, and improving the proper fitting of shoes are all important measures to decrease this common source of foot pain. Modification of footwear includes shoes with a raised heel and better arch support. Shoe orthotics recommended by a healthcare professional are often very helpful in conjunction with exercises to increase strength of the foot muscles and arch. The orthotic prevents excess pronation and lengthening of the plantar fascia and continued tearing of this structure. To aid in this reduction of inflammation, applying ice for 10-15 minutes after activities and use of anti-inflammatory medication can be helpful. Physical therapy can be beneficial with the use of heat modalities, such as ultrasound that creates a deep heat and reduces inflammation. If the pain caused by inflammation is constant, keeping the foot raised above the heart and/or compressed by wrapping with an ace bandage will help. Corticosteroid injections are also frequently used to reduce pain and inflammation. Taping can help speed the healing process by protecting the fascia from reinjury, especially during stretching and walking.
Surgical Treatment
When chronic heel pain fails to respond to conservative treatment, surgical treatment may be necessary. Heel surgery can provide relief of pain and restore mobility. The type of procedure used is based on examination and usually consists of releasing the excessive tightness of the plantar fascia, called a plantar fascia release. Depending on the presence of excess bony build up, the procedure may or may not include removal of heel spurs. Similar to other surgical interventions, there are various modifications and surgical enhancements regarding surgery of the heel.
Symptoms Of Bursitis Of The Foot
Overview
Whenever tissues rub against one another, a bursa forms to allow for smooth gliding. A bursa is a fluid-filled sac and occurs normally throughout the body. Only a few cell layers thick, a bursa is filled with a lubricating fluid. However, when irritated, a bursa can become markedly thickened and painful. This is often referred to as bursitis. The retrocalcaneal bursa is positioned to allow the Achilles tendon to glide over the back part (posterior aspect) of the heel bone. When this bone becomes enlarged, inflammation of the retrocalcaneal bursa occurs. This inflammation results in exquisite tenderness along the posterior aspect of the heel.
Causes
A bursa acts as a cushion and lubricant between tendons or muscles sliding over bone. There are bursas around most large joints in the body, including the ankle. The retrocalcaneal bursa is located in the back of the ankle by the heel. It is where the large Achilles tendon connects the calf muscles to the heel bone. Repeated or too much use of the ankle can cause this bursa to become irritated and inflamed. Possible causes are too much walking, running, or jumping. This condition is usually linked to Achilles tendinitis. Sometimes retrocalcaneal bursitis may be mistaken for Achilles tendinitis. Risks for this condition include starting an aggressive workout schedule, or suddenly increasing activity level without the right conditioning.
Symptoms
Medical experts strongly recommend that you consult a doctor if you have any of the symptoms below. Disabling joint pain that prevents you from doing your daily activities. Pain that lasts for more than two weeks. Excessive swelling, redness, bruising or a rash around the painful joint. Sharp or shooting pain, especially when you exercise or do something more strenuous. A fever. Any of the above could be a sign of infection, a condition such as arthritis or a more serious injury such as a tendon tear that may require medical attention.
Diagnosis
When a patient has pain in a joint, a careful physical examination is needed to determine what type of movement is affected and if there is any swelling present. Bursitis will not show up on x-rays, although sometimes there are also calcium deposits in the joint that can be seen. Inserting a thin needle into the affected bursa and removing (aspirating) some of the synovial fluid for examination can confirm the diagnosis. In most cases, the fluid will not be clear. It can be tested for the presence of microorganisms, which would indicate an infection, and crystals, which could indicate gout. In instances where the diagnosis is difficult, a local anesthetic (a drug that numbs the area) is injected into the painful spot. If the discomfort stops temporarily, then bursitis is probably the correct diagnosis.
Non Surgical Treatment
Conservative treatment includes the use of shoe supports (either a heel raise or a donut-shaped heel cushion) and a limited number of local corticosteroid injections (usually up to three per year). Changing the type of footwear may be essential.
Surgical Treatment
Bursectomy is a surgical procedure used to remove an inflamed or infected bursa, which is a fluid-filled sac that reduces friction between tissues of the body. Because retrocalcaneal bursitis can cause chronic inflammation, pain and discomfort, bursectomy may be used as a treatment for the condition when it is persistent and cannot be relived with other treatments. During this procedure, a surgeon makes small incisions so that a camera may be inserted into the joint. This camera is called an arthroscope. Another small incision is made so that surgical instruments can be inserted to remove the inflamed bursa.
Whenever tissues rub against one another, a bursa forms to allow for smooth gliding. A bursa is a fluid-filled sac and occurs normally throughout the body. Only a few cell layers thick, a bursa is filled with a lubricating fluid. However, when irritated, a bursa can become markedly thickened and painful. This is often referred to as bursitis. The retrocalcaneal bursa is positioned to allow the Achilles tendon to glide over the back part (posterior aspect) of the heel bone. When this bone becomes enlarged, inflammation of the retrocalcaneal bursa occurs. This inflammation results in exquisite tenderness along the posterior aspect of the heel.
Causes
A bursa acts as a cushion and lubricant between tendons or muscles sliding over bone. There are bursas around most large joints in the body, including the ankle. The retrocalcaneal bursa is located in the back of the ankle by the heel. It is where the large Achilles tendon connects the calf muscles to the heel bone. Repeated or too much use of the ankle can cause this bursa to become irritated and inflamed. Possible causes are too much walking, running, or jumping. This condition is usually linked to Achilles tendinitis. Sometimes retrocalcaneal bursitis may be mistaken for Achilles tendinitis. Risks for this condition include starting an aggressive workout schedule, or suddenly increasing activity level without the right conditioning.
Symptoms
Medical experts strongly recommend that you consult a doctor if you have any of the symptoms below. Disabling joint pain that prevents you from doing your daily activities. Pain that lasts for more than two weeks. Excessive swelling, redness, bruising or a rash around the painful joint. Sharp or shooting pain, especially when you exercise or do something more strenuous. A fever. Any of the above could be a sign of infection, a condition such as arthritis or a more serious injury such as a tendon tear that may require medical attention.
Diagnosis
When a patient has pain in a joint, a careful physical examination is needed to determine what type of movement is affected and if there is any swelling present. Bursitis will not show up on x-rays, although sometimes there are also calcium deposits in the joint that can be seen. Inserting a thin needle into the affected bursa and removing (aspirating) some of the synovial fluid for examination can confirm the diagnosis. In most cases, the fluid will not be clear. It can be tested for the presence of microorganisms, which would indicate an infection, and crystals, which could indicate gout. In instances where the diagnosis is difficult, a local anesthetic (a drug that numbs the area) is injected into the painful spot. If the discomfort stops temporarily, then bursitis is probably the correct diagnosis.
Non Surgical Treatment
Conservative treatment includes the use of shoe supports (either a heel raise or a donut-shaped heel cushion) and a limited number of local corticosteroid injections (usually up to three per year). Changing the type of footwear may be essential.
Surgical Treatment
Bursectomy is a surgical procedure used to remove an inflamed or infected bursa, which is a fluid-filled sac that reduces friction between tissues of the body. Because retrocalcaneal bursitis can cause chronic inflammation, pain and discomfort, bursectomy may be used as a treatment for the condition when it is persistent and cannot be relived with other treatments. During this procedure, a surgeon makes small incisions so that a camera may be inserted into the joint. This camera is called an arthroscope. Another small incision is made so that surgical instruments can be inserted to remove the inflamed bursa.