Over-Pronation Of The Feet Causes
Pronation is the normal movement the foot makes to absorb the impact from walking or running. It occurs once the heel strikes the ground and the foot disperses the impact, stretching and flattening the arch as the foot rolls inward. Supination is the opposite motion of pronation. The foot supinates, or rolls on its outer edge, to help with stability as we walk or run. A reasonable amount of pronation is necessary for the foot to function properly. However, when the foot arch remains flat and the foot rolls inward too much one may have excessive pronation or overpronation. This medical condition can result from continually straining the feet and wearing footwear that lacks sufficient foot arch support.

Causes
Unless there is a severe, acute injury, overpronation develops as a gradual biomechanical distortion. Several factors contribute to developing overpronation, including tibialis posterior weakness, ligament weakness, excess weight, pes planus (flat foot), genu valgum (knock knees), subtalar eversion, or other biomechanical distortions in the foot or ankle. Tibialis posterior weakness is one of the primary factors leading to overpronation. Pronation primarily is controlled by the architecture of the foot and eccentric activation of the tibialis posterior. If the tibialis posterior is weak, the muscle cannot adequately slow the natural pronation cycle.
Symptoms
Because pronation is a twisting of the foot, all of the muscles and tendons which run from the leg and ankle into the foot will be twisted. In over-pronation, resulting laxity of the soft tissue structures of the foot and loosened joints cause the bones of the feet shift. When this occurs, the muscles which attach to these bones must also shift, or twist, in order to attach to these bones. The strongest and most important muscles that attach to our foot bones come from our lower leg. So, as these muscles course down the leg and across the ankle, they must twist to maintain their proper attachments in the foot. Injuries due to poor biomechanics and twisting of these muscles due to over-pronation include: shin splints, Achilles Tendonitis, generalized tendonitis, fatigue, muscle aches and pains, cramps, ankle sprains, and loss of muscular efficiency (reducing walking and running speed and endurance). Foot problems due to over-pronation include: bunions, heel spurs, plantar fasciitis, fallen and painful arches, hammer toes, and calluses.
Diagnosis
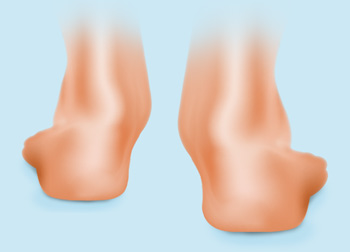
People who overpronate have flat feet or collapsed arches. You can tell whether you overpronate by wetting your feet and standing on a dry, flat surface. If your footprint looks complete, you probably overpronate. Another way to determine whether you have this condition is to simply look at your feet when you stand. If there is no arch on the innermost part of your sole, and it touches the floor, you likely overpronate. The only way to truly know for sure, however, is to be properly diagnosed by a foot and ankle specialist.
Non Surgical Treatment
No matter what the cause in your case, over pronation can be remedied in several ways. Those who are overweight should consider permanently losing weight to naturally alleviate pressure on the ligaments and heel of the foot. Also, you should consult a podiatrist to examine your posture and movement habits. You may be reinjuring yourself due to poor alignment without even knowing it. If you also have lower back problems, this could be a sign of over pronation as a result of misalignment.
Surgical Treatment
Hyperpronation can only be properly corrected by internally stabilizing the ankle bone on the hindfoot bones. Several options are available. Extra-Osseous TaloTarsal Stabilization (EOTTS) There are two types of EOTTS procedures. Both are minimally invasive with no cutting or screwing into bone, and therefore have relatively short recovery times. Both are fully reversible should complications arise, such as intolerance to the correction or prolonged pain. However, the risks/benefits and potential candidates vary. Subtalar Arthroereisis. An implant is pushed into the foot to block the excessive motion of the ankle bone. Generally only used in pediatric patients and in combination with other procedures, such as tendon lengthening. Reported removal rates vary from 38% - 100%, depending on manufacturer. HyProCure Implant. A stent is placed into a naturally occurring space between the ankle bone and the heel bone/midfoot bone. The stent realigns the surfaces of the bones, allowing normal joint function. Generally tolerated in both pediatric and adult patients, with or without adjunct soft tissue procedures. Reported removal rates, published in scientific journals vary from 1%-6%.
Calcaneal Apophysitis In Adolescents
Sever?s Disease is one of the most common overuse sports injuries in the U.S. It may not receive the street cred that plantar fasciitis gets, but this painful condition affecting the heel routinely affects child athletes, usually from eight to thirteen years of age, right when the bones are coming together. The pounding force causes inflammation between the bones, according to YNN, as well as injury to the growth plates themselves. While the ?disease? classification may sound scary, it?s actually a quite normal overuse sports injury that does not typically persist into adulthood.
Causes
During the growth spurt of early puberty, the heel bone (also called the calcaneus) sometimes grows faster than the leg muscles and tendons. This can cause the muscles and tendons to become very tight and overstretched, making the heel less flexible and putting pressure on the growth plate. The Achilles tendon (also called the heel cord) is the strongest tendon that attaches to the growth plate in the heel. Over time, repeated stress (force or pressure) on the already tight Achilles tendon damages the growth plate, causing the swelling, tenderness, and pain of Sever's disease. Such stress commonly results from physical activities and sports that involve running and jumping, especially those that take place on hard surfaces, such as track, basketball, soccer, and gymnastics.
Symptoms
If your child has any of the following symptoms, call your pediatrician for an evaluation. Heel pain that begins after starting a new sports season or a new sport. Walking with a limp or on tiptoes. Pain that increases with running or jumping. Heel tendon that feels tight. Pain when you squeeze the child's heel near the back. Pain in one or both heels.
Diagnosis
This can include physical examination and x-ray evaluation. X-rays may show some increased density or sclerosis of the apophysis (island of bone on the back of the heel). This problem may be on one side or bilateral.
Non Surgical Treatment
The immediate goal of treatment is pain relief. Because symptoms generally worsen with activity, the main treatment for Sever's disease is rest, which helps to relieve pressure on the heel bone, decreasing swelling and reducing pain. As directed by the doctor, a child should cut down on or avoid all activities that cause pain until all symptoms are gone, especially running barefoot or on hard surfaces because hard impact on the feet can worsen pain and inflammation. The child might be able to do things that do not put pressure on the heel, such as swimming and biking, but check with a doctor first.
Surgical Treatment
The surgeon may select one or more of the following options to treat calcaneal apophysitis. Reduce activity. The child needs to reduce or stop any activity that causes pain. Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue. Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile. Often heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis, or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.
Foot Arch Pain
Pain or strain in your foot arches is a common sports injury and often linked to inflammation of the plantar fascia, the shock absorption ligament along the bottom of each foot. The pain can also highlight underlying issues to do with the structure of your arches.

Causes
Also known as pes planus, this is when the arch of the foot collapses completely dropping the whole sole of the foot down to the ground. Flat feet are a common cause of foot arch pain. Babies are born with flat feet and as they grow, the foot arches should gradually form, but in approximately 30% of the population, they never do. They can also develop later in life, due to illness, pregnancy, injury, excessive stress on the feet or as part of the aging process. Many people who have flat feet don?t complain of any accompanying symptoms, but some develop foot arch pain, or problems further up the leg such as knee pain or back pain. They may find their feet tire quickly when they are standing or walking, and that it is difficult to rise up onto their tiptoes. Someone who is experiencing pain on the bottom of the foot or elsewhere due to their flat feet can benefit from exercises and orthotics (specially designed insoles to correct the foot position) as well as walking barefoot rather than in shoes. A quick test to see if you have flat feet is to put your foot in a tray of water and then place it on a smooth level surface e.g. thick paper. Have a look at your footprint, the more of the sole of the foot that you can see, the flatter your foot.
Symptoms
Intense heel pain, especially first thing in the morning and after a long day. Difficulty walking or standing for long periods without pain. Generally, the sharp pain associated with plantar fasciitis is localized to the heel, but it can spread forward along the arch of the foot and back into the Achilles tendon. While severe cases can result in chronic pain that lasts all day, the most common flare ups occur first thing in the morning, making those first steps out of bed a form of torture, and in the evening after having spent a day on your feet. Overpronation (a foot that naturally turns too far inward), high arches, and flat feet (fallen arches) can all cause similar arch pain. In these cases, however, the pain is more likely to continue throughout the day rather than being worst in the morning.
Diagnosis
Your doctor may order imaging tests to help make sure your heel pain is caused by plantar fasciitis and not another problem. X-rays provide clear images of bones. They are useful in ruling out other causes of heel pain, such as fractures or arthritis. Heel spurs can be seen on an x-ray. Other imaging tests, such as magnetic resonance imaging (MRI) and ultrasound, are not routinely used to diagnose plantar fasciitis. They are rarely ordered. An MRI scan may be used if the heel pain is not relieved by initial treatment methods.
Non Surgical Treatment
If it is flat feet, then you'd seek professional advice and maybe need orthotics, or arch supports to prevent the pressures and to stop the pain. One of the other reasons you can get pain in this area of the foot is plantar fasciitis. The plantar fascia is a membrane that is inside of the skin and attaches to the heel bone here. It divides into three bands that go out of the foot here: the outer band, the central band, and the medial band here. Often, from impact, you get an inflammation of that attachment to the heel bone and this can often spread up the medial band and this is another way of getting pain in that arch. Now, the way to treat that is also using arch supports but also heel cushions, better soled shoes to prevent the pressure. These things normally disappear after a year, 18 months. Plantar fasciitis is easier to treat because it's not a long term problem. If you do need arch support, something like this would be very good for both problems.

Surgical Treatment
Surgery is considered only after 12 months of aggressive nonsurgical treatment. Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the plantar fascia, this procedure is useful for patients who still have difficulty flexing their feet, despite a year of calf stretches. In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope, an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs. Complication rates for gastrocnemius recession are low, but can include nerve damage. Plantar fascia release. If you have a normal range of ankle motion and continued heel pain, your doctor may recommend a partial release procedure. During surgery, the plantar fascia ligament is partially cut to relieve tension in the tissue. If you have a large bone spur, it will be removed, as well. Although the surgery can be performed endoscopically, it is more difficult than with an open incision. In addition, endoscopy has a higher risk of nerve damage. The most common complications of release surgery include incomplete relief of pain and nerve damage. Most patients have good results from surgery. However, because surgery can result in chronic pain and dissatisfaction, it is recommended only after all nonsurgical measures have been exhausted.
Prevention
Stretch and strengthen important muscles in your feet, ankles and legs in order to guard against future strain. Make sure to acquire suitable arch supports and inserts if necessary, and that your shoes are shock absorbent and in good condition. Wearing tattered shoes provides no protection, and runners should replace their footwear before exceeding 500 miles of usage. Athletes new to arch supports should gradually build their training routine, allowing their feet to become accustomed to a new stance.
Stretching Exercises
People with flexible feet who develop fallen arches may benefit from foot strengthening exercises, notes the Nicholas Institute of Sports Medicine and Athletic Trauma. Standing on a towel in bare feet and grasping the material with the toes is an easy foot-strengthening exercise that can be done at home. Standing on one leg while arching and releasing the foot may also prove useful. Doctors may prescribe gentle stretching exercises for the foot and ankle tendons.
What Are The Leading Causes Of Posterior Tibial Tendon Dysfunction ?
Overview
Adult-acquired flatfoot or collapsed arch occurs because the large tendon on the inside of the ankle - the posterior tibial tendon - becomes stretched out and no longer supports the foot?s arch. In many cases, the condition worsens and and the tendon thickens, becoming painful, especially during activities. Flatfoot or collapsed arch is also known as posterior tibial tendon dysfunction. This condition is different than having flat feet since birth (known as congenital flatfoot), although sometimes these patients develop similar symptoms and require similar treatments. 
Causes
Overuse of the posterior tibial tendon is often the cause of PTTD. In fact, the symptoms usually occur after activities that involve the tendon, such as running, walking, hiking, or climbing stairs.
Symptoms
The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
Looking at the patient when they stand will usually demonstrate a flatfoot deformity (marked flattening of the medial longitudinal arch). The front part of the foot (forefoot) is often splayed out to the side. This leads to the presence of a ?too many toes? sign. This sign is present when the toes can be seen from directly behind the patient. The gait is often somewhat flatfooted as the patient has the dysfunctional posterior tibial tendon can no longer stabilize the arch of the foot. The physician?s touch will often demonstrate tenderness and sometimes swelling over the inside of the ankle just below the bony prominence (the medial malleolus). There may also be pain in the outside aspect of the ankle. This pain originates from impingement or compression of two tendons between the outside ankle bone (fibula) and the heel bone (calcaneus) when the patient is standing.
Non surgical Treatment
There are many non-surgical options for the flatfoot. Orthotics, non-custom braces, shoe gear changes and custom braces are all options for treatment. A course of physical therapy may be prescribed if tendon inflammation is part of the problem. Many people are successfully treated with non-surgical alternatives. 
Surgical Treatment
If cast immobilization fails, surgery is the next alternative. Treatment goals include eliminating pain, halting deformity progression and improving mobility. Subtalar Arthroereisis, 15 minute outpatient procedure, may correct flexible flatfoot deformity (hyperpronation). The procedure involves placing an implant under the ankle joint (sinus tarsi) to prevent abnormal motion. Very little recovery time is required and it is completely reversible if necessary. Ask your Dallas foot doctor for more information about this exciting treatment possibility.
Which Are The Main Causes Of Posterior Tibial Tendon Dysfunction (PTTD) ?
Overview
Some people have always had flat feet from a young age. Unfortunately as people reach their fifties they will suddenly have one foot with a flatter arch than the other foot. This situation is termed adult acquired flatfoot. Adult acquired flatfoot is a painful condition occurring in one foot. The common patient profile is a female over the age of 50 with pre-existing flatfeet, high blood pressure, high cholesterol, diabetes and obesity. All of these underlying problems will lead to a weakening of the support structures of the arch. If you have adult acquired flat foot you will not be able to lift your heel off the ground while standing on one leg. Adult acquired flatfoot may develop due to trauma or degeneration of major tendons ankle & foot. Weakness or paralysis of leg muscles can also create a flatfoot deformity. 
Causes
There are numerous causes of acquired adult flatfoot, including fracture or dislocation, tendon laceration, tarsal coalition, arthritis, neuroarthropathy, neurologic weakness, and iatrogenic causes. The most common cause of acquired adult flatfoot is posterior tibial tendon dysfunction.
Symptoms
Initially, flatfoot deformity may not present with any symptoms. However, overtime as the tendon continues to function in an abnormal position, people with fallen arches will begin to have throbbing or sharp pain along the inside of the arch. Once the tendon and soft tissue around it elongates, there is no strengthening exercises or mechanism to shorten the tendon back to a normal position. Flatfoot can also occur in one or both feet. If the arch starts to slowly collapse in one foot and not the other, posterior tibial dysfunction (PTTD) is the most likely cause. People with flatfoot may only have pain with certain activities such as running or exercise in the early phase of PTTD. Pain may start from the arch and continue towards the inside part of the foot and ankle where the tendon courses from the leg. Redness, swelling and increased warmth may also occur. Later signs of PTTD include pain on the outside of the foot from the arch collapsing and impinging other joints. Arthritic symptoms such as painful, swollen joints in the foot and ankle may occur later as well due to the increased stress on the joints from working in an abnormal position for a long period of time.
Diagnosis
The diagnosis of posterior tibial tendon dysfunction and AAFD is usually made from a combination of symptoms, physical exam and x-ray imaging. The location of pain, shape of the foot, flexibility of the hindfoot joints and gait all may help your physician make the diagnosis and also assess how advanced the problem is.
Non surgical Treatment
Nonoperative treatment of posterior tibial tendon dysfunction can be successful with the Arizona AFO brace, particularly when treatment is initiated in the early stages of the disease. This mandates that the orthopedist has a high index of suspicion when evaluating patients to make an accurate diagnosis. Although there is a role for surgical management of acquired flat feet, a well-fitted, custom-molded leather and polypropylene orthosis can be effective at relieving symptoms and either obviating or delaying any surgical intervention. In today's climate of patient satisfaction directed health care, a less invasive treatment modality that relieves pain may prove to be more valuable than similar pain relief that is obtained after surgery. Questions regarding the long-term results of bracing remain unanswered. Future studies are needed to determine if disease progression and arthrosis occur despite symptomatic relief with a brace. Furthermore, age- and disease stage-matched control groups who are randomized to undergo surgery or bracing are necessary to compare these different treatment modalities. 
Surgical Treatment
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Surgical treatment may include repairing the tendon, tendon transfers, realigning the bones of the foot, joint fusions, or both. Dr. Piccarelli will determine the best approach for your specific case. A variety of surgical techniques is available to correct flexible flatfoot. Your case may require one procedure or a combination of procedures. All of these surgical techniques are aimed at relieving the symptoms and improving foot function. Among these procedures are tendon transfers or tendon lengthening procedures, realignment of one or more bones, or insertion of implant devices. Whether you have flexible flatfoot or PTTD, to select the procedure or combination of procedures for your particular case, Dr. Piccarelli will take into consideration the extent of your deformity based on the x-ray findings, your age, your activity level, and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
Achilles Tendonitis Recovery Exercises
 The Achilles tendon is the largest tendon in the body. It is formed by the merging together of the upper calf muscles and inserts into the back of the heel bone. Its blood supply comes from the muscles above and the bony attachment below. The blood supply is limited at the ?watershed? zone approximately 1 to 4 inches above the insertion into the heel bone. Paratendonitis and tendinosis develop in the same area. Achilles tendinitis implies an inflammatory response, but this is very limited because there is little blood supply to the Achilles tendon. More appropriate descriptions are inflammation of the surrounding sheath (paratenonitis), degeneration within the substance of the tendon (tendinosis) or a combination of the two.
The Achilles tendon is the largest tendon in the body. It is formed by the merging together of the upper calf muscles and inserts into the back of the heel bone. Its blood supply comes from the muscles above and the bony attachment below. The blood supply is limited at the ?watershed? zone approximately 1 to 4 inches above the insertion into the heel bone. Paratendonitis and tendinosis develop in the same area. Achilles tendinitis implies an inflammatory response, but this is very limited because there is little blood supply to the Achilles tendon. More appropriate descriptions are inflammation of the surrounding sheath (paratenonitis), degeneration within the substance of the tendon (tendinosis) or a combination of the two.
Causes
Achilles tendonitis occurs in sports such as running, jumping, dancing and tennis. Other risk factors include participation in a new sporting activity or increasing the intensity of participation. Poor running technique, excessive pronation of the foot and poorly fitting footwear may contribute. In cyclists, the problem may be a low saddle, which causes extra dorsiflexion of the ankle when pedalling. Quinolone antibiotics (eg, ciprofloxacin, ofloxacin) can cause inflammation of tendons and predispose them to rupture.
Symptoms
A symptom is something the patient feels and reports, while a sign is something other people, such as a doctor, detect. For example, pain is a symptom, while a rash is a sign. The most typical symptom of Achilles tendinitis is a gradual buildup of pain that deteriorates with time. With Achilles tendinitis, the Achilles tendon may feel sore a few centimeters above where it meets the heel bone. Other possible signs and symptoms of Achilles tendinitis are, the Achilles tendon feels sore a few centimeters above where it meets the heel bone, lower leg feels stiff or lower leg feels slow and weak. Slight pain in the back of the leg that appears after running or exercising, and worsens, pain in the Achilles tendon that occurs while running or a couple of hours afterwards. Greater pain experienced when running fast (such as sprinting), for a long time (such as cross country), or even when climbing stairs. The Achilles tendon swells or forms a bump or the Achilles tendon creaks when touched or moved. Please note that these symptoms, and others similar can occur in other conditions, so for an accurate diagnosis, the patient would need to visit their doctor.
Diagnosis
When diagnosing Achilles tendinitis, a doctor will ask the patient a few questions about their symptoms and then perform a physical examination. To perform a physical exam on the Achilles tendon, the doctor will lightly touch around the back of the ankle and tendon to locate the source of the pain or inflammation. They will also test the foot and ankle to see if their range of motion and flexibility has been impaired. The doctor might also order an imaging test to be done on the tendon. This will aid in the elimination of other possible causes of pain and swelling, and may help the doctor assess the level of damage (if any) that has been done to the tendon. Types of imaging tests that could be used for diagnosing Achilles tendinitis are MRI (Magnetic resonance imaging), X-ray, Ultrasound.
Nonsurgical Treatment
The first thing to do is to cut back your training. If you are working out twice a day, change to once a day and take one or two days off per week. If you are working out every day cut back to every other day and decrease your mileage. Training modification is essential to treatment of this potentially long lasting problem. You should also cut back on hill work and speed work. Post running ice may also help. Be sure to avoid excessive stretching. The first phase of healing should be accompanied by relative rest, which doesn't necessarily mean stopping running, but as I am emphasizing, a cut back in training. If this does not help quickly, consider the use of a 1/4 inch heel lift can also help. Do not start worrying if you will become dependent on this, concentrate on getting rid of the pain. Don't walk barefoot around your house, avoid excessively flat shoes, such as "sneakers", tennis shoes, cross trainers, etc. In office treatment would initially consist of the use of the physical therapy modalities of electrical stimulation, (HVGS, high voltage galvanic stimulation), and ultrasound. Your sports medicine physician should also carefully check your shoes. A heel lift can also be used and control of excessive pronation by taping can also be incorporated into a program of achilles tendonitis rehabilitation therapy. Orthotics with a small heel lift are often helpful.

Surgical Treatment
If several months of more-conservative treatments don't work or if the tendon has torn, your doctor may suggest surgery to repair your Achilles tendon.
Prevention
Warm up slowly by running at least one minute per mile slower than your usual pace for the first mile. Running backwards during your first mile is also a very effective way to warm up the Achilles, because doing so produces a gentle eccentric load that acts to strengthen the tendon. Runners should also avoid making sudden changes in mileage, and they should be particularly careful when wearing racing flats, as these shoes produce very rapid rates of pronation that increase the risk of Achilles tendon injury. If you have a tendency to be stiff, spend extra time stretching. If you?re overly flexible, perform eccentric load exercises preventively. Lastly, it is always important to control biomechanical alignment issues, either with proper running shoes and if necessary, stock or custom orthotics.
Working With Fallen Arches

Flat feet can develop as an adult ("adult acquired flatfoot") due to injury, illness, unusual or prolonged stress to the foot, faulty biomechanics,[5] or as part of the normal aging process. Flat feet can also occur in pregnant women as a result of temporary changes, due to increased elastin (elasticity) during pregnancy. However, if developed by adulthood, flat feet generally remain flat permanently.
Causes
Fallen arches may be caused by a number of causes, including increased elastin during pregnancy, arthritis, injury, excessive stress on the foot, fused bones in the foot, or an extra bone. They may cause not only foot pain, but also pain in the legs, knees, and back and a loss of mobility. The condition is most often treated with orthotics, structures placed in the shoes to support the feet, but this may not be enough for severe cases. Exercises to strengthen and rebuild the arches can also be helpful. Surgery is sometimes the best method of treatment, as it can completely rebuild the arches and has lasting results, but it is quite expensive and considered a last resort.
Symptoms
Flat feet don't usually cause problems, but they can put a strain on your muscles and ligaments (ligaments link two bones together at a joint). This may cause pain in your legs when you walk. If you have flat feet, you may experience pain in any of the following areas, the inside of your ankle, the arch of your foot, the outer side of your foot, the calf, the knee, hip or back. Some people with flat feet find that their weight is distributed unevenly, particularly if their foot rolls inwards too much (overpronates). If your foot overpronates, your shoes are likely to wear out quickly. Overpronation can also damage your ankle joint and Achilles tendon (the large tendon at the back of your ankle).
Diagnosis
Many medical professionals can diagnose a flat foot by examining the patient standing or just looking at them. On going up onto tip toe the deformity will correct when this is a flexible flat foot in a child with lax joints. Such correction is not seen in the adult with a rigid flat foot. An easy and traditional home diagnosis is the "wet footprint" test, performed by wetting the feet in water and then standing on a smooth, level surface such as smooth concrete or thin cardboard or heavy paper. Usually, the more the sole of the foot that makes contact (leaves a footprint), the flatter the foot. In more extreme cases, known as a kinked flatfoot, the entire inner edge of the footprint may actually bulge outward, where in a normal to high arch this part of the sole of the foot does not make contact with the ground at all.
Non Surgical Treatment
What we want to do is support the arch and maintain it in that curved position. So what you want is to bring the foot into a position where you hold and support the arch so you can get that correct heel-midfoot-big toe contact. You would achieve that with a level of arch support. People will take different levels of support, if you?re somebody who has movement in your arch, a strong level of support will hold and maintain you whereas if you?re someone whose arch has collapsed it could need more support and a level of correction built into the support to realign you. If you think of it, when your arch drops, it affects your foot but it also has a biomechanical effect on the rest of the body. But nothing that can?t be solved.
Surgical Treatment

Surgery for flat feet is separated into three kinds: soft tissue procedures, bone cuts, and bone fusions. Depending on the severity of the flat foot, a person?s age, and whether or not the foot is stiff determines just how the foot can be fixed. In most cases a combination of procedures are performed. With flexible flat feet, surgery is geared at maintaining the motion of the foot and recreating the arch. Commonly this may involve tendon repairs along the inside of the foot to reinforce the main tendon that lifts the arch. When the bone collapse is significant, bone procedures are included to physically rebuild the arch, and realign the heel. The presence of bunions with flat feet is often contributing to the collapse and in most situations requires correction. With rigid flat feet, surgery is focused on restoring the shape of the foot through procedures that eliminate motion. In this case, motion does not exist pre-operatively, so realigning the foot is of utmost importance. The exception, are rigid flat feet due to tarsal coalition (fused segment of bone) in the back of the foot where freeing the blockage can restore function.